
Writer:
Prof. Dr. Satish Kumar Panda, MD (Ay), PhD
Principal, Kritika Ayurvedic Medical College & Hospital, Bareilly, Uttar Pradesh.
Table of Contents
- Definition & Pathophysiology
- Etiology (Causes of Cirrhosis)
- Clinical Features
- Diagnosis & Investigations
- Child-Pugh & MELD Scoring
- Complications
- Management & Treatment
- Prognosis
- Key Takeaways & Mnemonics
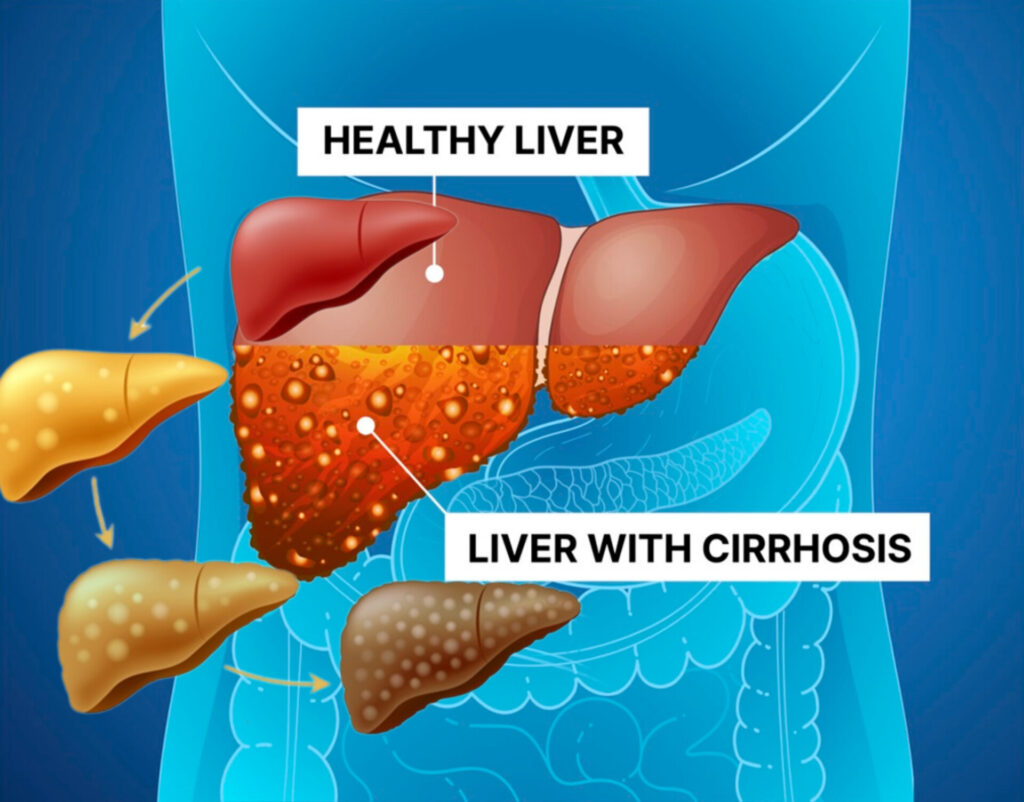
1. Definition & Pathophysiology
What is Liver Cirrhosis?
- Cirrhosis is the end-stage of chronic liver disease, characterized by:
- Fibrosis (scar tissue replacing healthy liver parenchyma).
- Regenerative nodules (required for diagnosis).
- Portal hypertension (increased pressure in the portal vein).
Key Pathophysiological Changes
- Hepatocyte Injury → Chronic inflammation (e.g., viral hepatitis, alcohol).
- Activation of Stellate Cells → Excessive collagen deposition (fibrosis).
- Distorted Liver Architecture →
- Impaired liver function (↓ detoxification, ↓ protein synthesis).
- Increased vascular resistance → Portal HTN.
- Compensated vs. Decompensated Cirrhosis
- Compensated: Liver functions normally despite fibrosis (asymptomatic or mild fatigue).
- Decompensated: Liver failure (jaundice, ascites, variceal bleeding, encephalopathy).
2. Etiology (Causes of Cirrhosis) – Mnemonic: “VW HAPPENS”
| Category | Specific Causes | Key Features |
|---|---|---|
| Viral Hepatitis | HCV, HBV, HDV | HCV most common worldwide; HBV linked to HCC. |
| Alcohol (ASH) | Chronic alcoholism | AST:ALT >2:1, ↑GGT, ↑MCV. |
| NASH | Obesity, diabetes | Metabolic syndrome, no alcohol history. |
| Autoimmune | PBC, PSC, AIH | PBC (AMA+), PSC (IBD association), AIH (ANA/ASMA+). |
| Genetic/Metabolic | Hemochromatosis, Wilson’s, A1AT | Hemochromatosis (↑ferritin), Wilson’s (Kayser-Fleischer rings). |
| Vascular | Budd-Chiari, PVT | Hepatic vein thrombosis (Budd-Chiari), portal vein obstruction. |
| Drugs/Toxins | Methotrexate, acetaminophen | Direct hepatotoxicity. |
3. Clinical Features
Early (Compensated) Cirrhosis
- Fatigue, weakness, weight loss.
- Physical signs:
- Palmar erythema, spider angiomas (↑estrogen).
- Dupuytren’s contracture (alcohol-related).
- Clubbing, leukonychia (hypoalbuminemia).
Late (Decompensated) Cirrhosis
| Complication | Symptoms/Signs |
|---|---|
| Portal HTN | Ascites, splenomegaly, varices (esophageal, rectal). |
| Ascites | Abdominal distension, shifting dullness. |
| Variceal Bleeding | Hematemesis, melena, shock. |
| Hepatic Encephalopathy | Confusion, asterixis, coma. |
| Hepatorenal Syndrome | Oliguria, ↑creatinine. |
| HCC (Hepatocellular Carcinoma) | RUQ mass, ↑AFP. |
4. Diagnosis & Investigations
Laboratory Tests
- LFTs: AST > ALT (alcohol/NASH), ↑bilirubin, ↓albumin.
- CBC: Thrombocytopenia (hypersplenism), anemia.
- Coagulation: Prolonged PT/INR (↓ clotting factors).
- Etiology-specific tests:
- Viral serology (HCV Ab, HBsAg).
- Autoantibodies (AMA for PBC, ANA/ASMA for AIH).
- Ferritin/TIBC (hemochromatosis), ceruloplasmin (Wilson’s).
Imaging
- Ultrasound: Nodular liver, ascites, splenomegaly.
- FibroScan (Elastography): Measures liver stiffness.
- CT/MRI: Detects HCC, vascular abnormalities.
Liver Biopsy (Gold Standard)
- Shows bridging fibrosis + regenerative nodules.
5. Child-Pugh & MELD Scoring (Prognosis)
Child-Pugh Score
| Parameter | 1 Point | 2 Points | 3 Points |
|---|---|---|---|
| Bilirubin (mg/dL) | <2 | 2-3 | >3 |
| Albumin (g/dL) | >3.5 | 2.8-3.5 | <2.8 |
| INR | <1.7 | 1.7-2.3 | >2.3 |
| Ascites | None | Mild | Severe |
| Encephalopathy | None | Grade 1-2 | Grade 3-4 |
- Class A (5-6): Good prognosis (85% 2-year survival).
- Class B (7-9): Moderate (60% survival).
- Class C (10-15): Poor (35% survival, transplant needed).
MELD Score
- Predicts 3-month mortality in cirrhosis.
- Formula:
MELD = 3.8 × ln(bilirubin) + 11.2 × ln(INR) + 9.6 × ln(creatinine) + 6.4- MELD ≥15: Indicates need for liver transplant.
6. Complications
| Complication | Key Features | Management |
|---|---|---|
| Variceal Bleeding | Hematemesis, shock | Band ligation, IV octreotide, NSBB (propranolol). |
| Ascites | Shifting dullness, abdominal distension | Salt restriction, spironolactone + furosemide. |
| SBP (Spontaneous Bacterial Peritonitis) | Ascitic fluid PMN >250 | IV cefotaxime. |
| Hepatic Encephalopathy | Confusion, asterixis | Lactulose, rifaximin. |
| Hepatorenal Syndrome | Oliguria, ↑Cr | Albumin + vasoconstrictors (terlipressin). |
| HCC | ↑AFP, liver mass | Surveillance (US every 6 months). |
7. Management & Treatment
General Approach
- Treat underlying cause:
- HCV: Direct-acting antivirals (sofosbuvir/velpatasvir).
- Alcohol: Abstinence.
- Autoimmune: Steroids (AIH), ursodeoxycholic acid (PBC).
- Monitor for complications (ascites, varices, HCC).
- Liver transplant for decompensated cirrhosis (MELD ≥15).
Symptomatic Management
- Ascites: Salt restriction + diuretics (spironolactone + furosemide).
- Varices: Non-selective beta-blockers (propranolol) + endoscopic banding.
- Encephalopathy: Lactulose (reduces ammonia), rifaximin.
8. Prognosis
- Compensated cirrhosis: 10-year survival ~50%.
- Decompensated cirrhosis: 2-year survival ~50%.
- Hepatorenal syndrome: Poor prognosis without transplant.
9. Key Takeaways & Mnemonics
Mnemonics
- Causes of Cirrhosis: “VW HAPPENS” (Viral, Wilson’s, Hemochromatosis, Alcohol, PBC/PSC, NASH, Storage diseases).
- AST:ALT Ratio >2:1 → Alcoholic hepatitis.
- SAAG ≥1.1 g/dL → Portal HTN-related ascites.
High-Yield Exam Points
- Kayser-Fleischer rings → Wilson’s disease.
- AMA+ → Primary Biliary Cholangitis (PBC).
- Spider angiomas + palmar erythema → Hyperestrogenism in cirrhosis.
- First-line for SBP → Cefotaxime.
Final Notes
- Cirrhosis is irreversible, but early intervention can slow progression.
- Screen for HCC (ultrasound + AFP every 6 months).
- Refer for transplant if decompensated (Child-Pugh C or MELD ≥15).
This guide covers everything a medical student needs for exams and clinical practice.
